

Healthcare providers today face a unique challenge. On one hand, patient care demands their full attention. Conversely, administrative tasks like billing, compliance, and insurance verifications slow them down. It is a balancing act. However, they cannot afford to get it wrong. A trusted medical billing system must do just that in an industry where mistakes are costly – in dollars and loss of a patient’s trust.
Medical billing is a minefield of errors, with Becker’s Hospital Review reporting that nearly 80% of claims contain mistakes. These errors lead to delays in claims processing, denied claims, and ultimately, lost revenues. In healthcare practice, these are not just headaches, but serious threats to financial stability. However, with the right medical billing software, providers can turn these challenges into opportunities.
In this guide, we focus on developing a medical billing system that automates core billing processes but, more importantly, addresses real-world problems. In terms of the content to be covered, we touch everything from core workflows and system integrations to reducing denial rates and ensuring compliance. More importantly, we will show you how a well-built system helps healthcare providers focus less on administration and more on what matters most: patients.
Why medical billing systems matter
Billing errors and inefficient processes can weaken a healthcare organization. They create bottlenecks, reduce revenue and frustrate patients. The following image highlights the key touchpoints a healthcare organization taps in medical billing. A well-constructed billing system changes that.
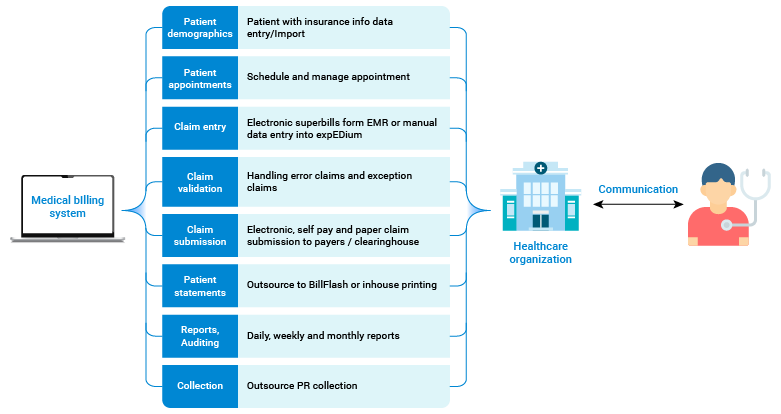
A healthcare organization’s routine tasks and responsibilities in medical billing without software assistance.
It ensures faster reimbursements, fewer claim rejections and a smoother overall revenue cycle. Undoubtedly, the following numbers from different estimates speak for themselves:
- U.S. hospitals lose $262 billion each year due to denied claims.
- Manual billing causes a 25-35-day delay in claim payments.
- Medical bills sometimes require 100+ fields to complete.
The numbers above paint a stark picture of the challenges manual medical billing systems face. Here are some more areas where manual touchpoints in a billing system led to inefficiency.
The issues with paper-based medical billing practices
For many years, medical billing was based on manual processes. Naturally, this is both highly inefficient and very cumbersome. For sophisticated health care, this paper-based approach quickly became the largest obstacle to medical practices.
Here are the key issues:
1. High error rates: Humans are fallible. We can make errors in coding, claims verification, or simple data entry. Manual data entry errors occur around 15% of the time. This leads to rejected claims and lost revenues.
2. Time-consuming tasks: There is verification of insurance and the process of denial, which is highly time-consuming. Based on estimates, healthcare providers spend 17 hours a week reworking denied claims.
3. Compliance risks: Billing regulations like HIPAA and ICD coding constantly change. Being manually compliant can lead to costly mistakes that could be considered compliance violations or fines.
4. Delayed payments: The average revenue cycle time in practices reliant on manual billing is 25-35 days. This long wait reduces cash flow, delaying payments and affecting financial health.
5. High operational costs: Maintaining a large billing department to manage manual processes adds to operational expenses. This reduces overall profit margins for healthcare providers.
6. Lack of scalability: As patient volumes grow, manual processes create backlogs. Scaling these outdated systems becomes nearly impossible.
7. Limited data insights: It is not easy to track performance or optimize workflows without automated analytics. Such practices can only take opportunities if they improve billing efficiency and accuracy.
When you look at the bigger picture, it becomes clear: manual processes make it harder to succeed. That is where medical billing software comes in – introducing automation that nullifies the error and maximizes efficiency.
Suggested: A healthcare provider cut manual data entry time by 40% using AI automation. Discover how your billing processes can achieve similar efficiencies. Read about the use cases of generative AI in the healthcare industry.
A step-by-step approach for building a medical billing system
Step 1: Map the core workflows
A well-designed medical billing system starts by using core billing workflows. These workflows constitute the heart and soul of the billing cycle, ensuring that the process flows without a hitch from when the patient walks to when the final payment check is cashed. Some of these include the following:
| Workflow | Purpose |
| Patient registration | Capture and validate patient information, including insurance, at first patient contact. |
| Insurance verification | Confirm in real time whether the patient’s policy will cover the treatment they seek. |
| Medical coding and claims | Relate the care to standard code recommendations for the medical providers (ICD and CPT) and make the claims based on the treatments offered. |
| Claims submission | Submit claims electronically to payers or through clearinghouses, reducing processing time and ensuring accuracy. |
| Claims tracking and denial | Track the progress of claims, quickly flag and fix denied claims, and resubmit them efficiently. |
| Payment posting | Log payments from insurers and patients, and ensure accounts reflect up-to-date balances. |
| Patient billing | Generate statements for patients, clearly outlining any outstanding balances, and offer online payment options for ease. |
Building your software around these workflows ensures that every step in the billing process is noticed. Each workflow contributes to smoother operations and better outcomes.
Step 2: Integrate with critical systems
Medical billing software cannot operate in isolation. It must play harmoniously with other healthcare systems to confirm accuracy and reduce redundant data entry. Here’s a look at the key integrations every billing system needs:
| System | Integration purpose |
| Electronic health records (EHR) | Sync patient care data to ensure accurate claim generation based on the services provided. |
| Insurance providers and clearinghouses | Enable real-time verification and claim submissions, reducing the chances of denial due to coverage issues. |
| Practice management systems (PMS) | Coordinate scheduling, administrative records and billing. It guarantees that all services are properly billed. |
| Telemedicine platforms | Capture and bill for virtual consultations, an increasingly important part of modern healthcare. |
According to an article in the Annals of Family Medicine, physicians spent over 50% of their time on their EHRs, documenting interferes of their interactions with patients as illustrated in the image below. The integration of such core system to the billing software lightens the stress and gives physicians time to focus on patients.
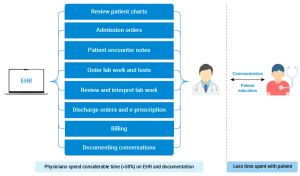
A medical billing system software needs all the data from an EHR
Imagine the spectrum of transformation the medical billing software can bring when it integrates with other critical systems. Automated data transfers eliminate repetitive tasks and reduce errors.
Step 3: User-friendly efficiency
A medical billing system must make it easy and not allow complexity. The software should be easy, efficient, reliable, and scalable.
- User interface: Design the system to be simple and user-friendly so that healthcare professionals can easily navigate. Errors and inefficiencies always create a steep learning curve.
- Automated workflows: Automate activities such as claim submissions and denial management so fewer manual inputs are required and error rates decrease significantly.
- Compliant-ready: Ensure the software is HIPAA compliant with all other regulatory requirements so that this does not become a “have to endure” costly penalty.
- Scalability: As a medical provider, when expanding the practice, billing needs to take care of more patients, increase complexity in billing, and still manage without performance problems associated with that increase.
Highlighting these aspects forms a system that supports long-term success for healthcare organizations.
Suggested: A healthcare organization streamlined its billing process with EHR migration to Microsoft 365 integration. See how this can simplify your medical billing software. Learn more about our approach.
Impact of automation on medical billing
Automation changes the way billing is done. It streamlines operations and reduces human error across critical areas. Let’s explore some specific processes where automation makes a big difference:
| Process | Manual approach | Automated solution |
| Insurance verification | Manually checks insurance eligibility, increasing the risk of denied claims. | Automate real time verification to ensure coverage before services are rendered. |
| Claim generation | Manually enters treatment data into claim forms, often leading to coding errors. | Automatically convert care into accurate claims with proper coding. |
| Denial management | Identify and correct denied claims through a laborious process that takes days or weeks. | Flag denied claims immediately and automatically suggest corrections, allowing quick resubmissions. |
| Patient billing | Send paper bills, often leading to delayed payments. | Automate patient statements and offer online payment options for faster and more convenient transactions. |
Automation is a powerful tool that can alleviate financial pressure, boost efficiency, reduce denial rates, and accelerate the revenue cycle. For instance, 32% of healthcare organizations that have embraced automation have seen a significant reduction in claim denials, leading to improved cash flow and patient satisfaction.
Maintaining a medical billing system
Once your system is live, understanding and addressing the key areas of maintenance is crucial for its long-term sustainability, efficiency, and security. Following are the key areas concerning:
- Compliance: It should be updated frequently with the latest rules and regulations. It may include HIPAA, ICD, etc. In case of non-compliance, the penalties may be very severe.
- Performance monitoring: The system’s performance must be periodically monitored to notice all inefficiency or potential bottlenecks.
- Data security: Regular security audits should be carried out to avoid data breaches and ensure that patient information is safe.
- Scalability: This should ensure that the performance does not degrade while the patient loads increase.
Suggested: A medical center reduced patient wait times and improved satisfaction with a mobile app. Explore how similar tools can enhance your medical billing efficiency.
Conclusion: The future of medical billing
Establishing an efficient medical billing system is more than just automating. It is a process that should be as beneficial to the consumer as it is to the provider. For healthcare organizations, the challenges of increasing costs, growing regulatory complexity, and high patient expectations are significant. Finding solutions to compete with these trends is a testament to any organization’s resilience and adaptability.
Your medical billing software can reduce errors, quicken payments, and display excellent overall patient satisfaction by focusing on the right workflows, integrations, and automation. For healthcare providers, this must translate to better financial health with more time to deliver quality care.
AI Workshop
Envision how your AI Journey can be in next 1-3 years from adoption and acceleration perspective.
Enroll NowNeed Help ?
We are here for you